Genetic polymorphism and current biotechnology approaches of therapeutic aspects within endometrial tumors
DOI:
https://doi.org/10.62063/rev-200153Keywords:
gynecological tumors, endometrial tumors, gene, single nucleotide polymporphism, biosensingAbstract
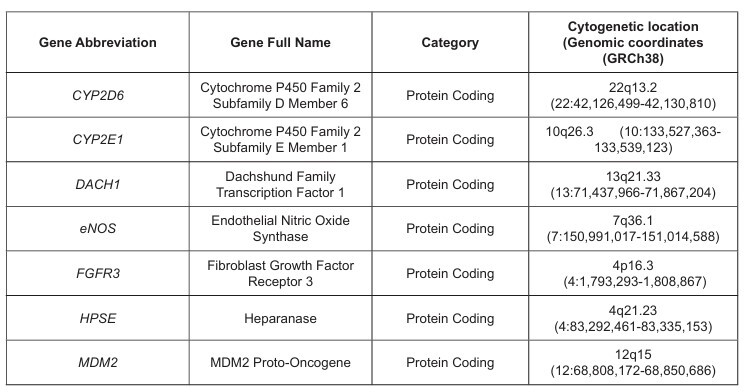
Among oncological diseases of women, gynecological diseases deserve special attention. Gynecological tumors are important to women's health throughout the world. Notably, gynecologic malignancies represent a prevalent category of cancers affecting women globally. Single nucleotide polymorphisms have emerged as a promising source of genetic information to better understand complex diseases such as cancer, in terms of etiology, interindividual differences and treatment response. In this review, we summarize some selected gene single nucleotide polymorphisms’ implication in gynecological cancer susceptibility/predisposition, as well as the potential to use such genetic markers for improved diagnosis and individualized treatment of gynecological cancers. Furthermore, this review explores the advances in biotechnology that have contributed to the management of gynecological tumors, in particular endometrial tumors, with a focus on molecular diagnostics, therapeutic innovations, and personalized medicine. It is critical to investigate the single nucleotide gene polymorphisms as sociated with gynecologic cancer susceptibility/predisposition as some of them might be utilized as useful molecular markers for assessing gynecologic cancer predisposition and might be further used for diagnosis and treatment modalities in individuals with similar single nucleotide polymorphism profile. Moreover, recent advancements in biosensing technologies, particularly nano-biosensors and microfluidic biosensors, have significantly enhanced the detection of gynecological tumor markers. Taken together, the revolution in cancer research, diagnosis, and treatment has been made possible by advances in biotechnology in recent decades.
References
Abena, T. (2023). Biosensors Technological Advancement and Their Biomedical, Agricultural, Environmental and Food Industrial Applications: A Review. International Journal on Food, Agriculture and Natural Resources, 4(3), 46–57. https://doi.org/10.46676/ij-fanres.v4i3.160
Ahmed, H. G., Bensumaidea, S. H., Alshammari, F. D., Alenazi, F. S. H., ALmutlaq, B. A., Alturkstani, M. Z., & Aladani, I. A. (2017). Prevalence of Human Papillomavirus subtypes 16 and 18 among Yemeni Patients with Cervical Cancer. Asian Pacific Journal of Cancer Prevention, 18(6), 1543-1547. https://doi.org/10.22034/APJCP.2017.18.6.1543
Arafa, M., Somja, J., Dehan, P., Kridelka, F., Goffin, F., Boniver, J., & Delvenne, P. (2010). Current concepts in the pathology and epigenetics of endometrial carcinoma. Pathology, 42(7), 613–617. https://doi.org/10.3109/00313025.2010.520307
Arciuolo, D., Travaglino, A., Raffone, A., Raimondo, D., Santoro, A., Russo, D., Varricchio, S., Casadio, P., Inzani, F., Seracchioli, R., Mollo, A., Mascolo, M., & Zannoni, G. F. (2022). TCGA molecular prognostic groups of endometrial carcinoma: current knowledge and future perspectives. International Journal of Molecular Sciences, 23(19), 11684. https://doi.org/10.3390/ijms231911684
Arora, T., Mullangi, S., & Lekkala, M. R. (2023). Ovarian Cancer. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK567760/
Baker-Rand, H., & Kitson, S. J. (2024). Recent advances in endometrial cancer prevention, early diagnosis and treatment. Cancers, 16(5), 1028. https://www.mdpi.com/2072-6694/16/5/1028
Banno, K., Yanokura, M., Iida, M., Masuda, K., & Aoki, D. (2014). Carcinogenic mechanisms of endometrial cancer: Involvement of genetics and epigenetics. The journal of obstetrics and gynaecology research, 40(8), 1957–1967. https://doi.org/10.1111/jog.12442
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A cancer journal for clinicians, 68(6), 394–424. https://doi.org/10.3322/caac.21492
Cai, J., Cui, K., Niu, F., Jin, T., Huang, S., Zhang, Y., & Bao, S. (2019). Genetics of IL6 polymorphisms: Case-control study of the risk of endometrial cancer. Molecular genetics & genomic medicine, 7(4), e00600. https://doi.org/10.1002/mgg3.600
Cao, H., Yang, S., Yu, X., & Xi, M. (2020). Correlation between heparanase gene polymorphism and susceptibility to endometrial cancer. Molecular genetics & genomic medicine, 8(10), e1257. https://doi.org/10.1002/mgg3.1257
Castellanos-Rubio, A., & Ghosh, S. (2019). Disease-Associated SNPs in Inflammation-Related lncRNAs. Frontiers in immunology, 10. https://doi.org/10.3389/fimmu.2019.00420
Cervical cancer. (n.d.). Retrieved December 4, 2023, from https://www.who.int/news-room/fact sheets/detail/cervical-cancer
Cheng, Y., Yang, L., Shi, G., Chen, P., Li, L., Fang, H., & Chen, C. (2021). Ninjurin 2 rs118050317 gene polymorphism and endometrial cancer risk. Cancer cell international, 21, 1-7. https://doi.org/10.1186/s12935-020-01646-5
Das, A. P., Chopra, M., & Agarwal, S. M. (2022). Prioritization and Meta-analysis of regulatory SNPs identified IL6, TGFB1, TLR9 and MMP7 as significantly associated with cervical cancer. Cytokine, 157, 155954. https://doi.org/10.1016/j.cyto.2022.155954
Datkhile, K. D., Durgawale, P. P., Gudur, R. A., Gudur, A. K., & Patil, S. R. (2022). CYP2D6 and CYP2E1 Gene Polymorphisms and their Association with Cervical Cancer Susceptibility: A Hospital Based Case-Control Study from South-Western Maharashtra. Asian pacific journal of cancer prevention : APJCP, 23(8), 2591–2597. https://doi.org/10.31557/APJCP.2022.23.8.2591
Deli, T., Orosz, M., & Jakab, A. (2020). Hormone replacement therapy in cancer survivors–review of the literature. Pathology & oncology research, 26(1), 63-78. https://doi.org/10.1007/s12253-01800569-x
Deng, Y., Zhang, Y., Zhou, M., Wu, B., & Zhou, J. (2023). Application of Biosensors in Detecting Breast Cancer Metastasis. Sensors, 23(21), 8813. https://doi.org/10.3390/s23218813
Dindere, M. E., Tanca, A., Rusu, M., Liehn, E. A., & Bucur, O. (2022). Intraoperative Tumor Detection Using Pafolacianine. International journal of molecular sciences, 23(21), 1–16. https://doi.org/10.3390/ijms232112842
Endometrial Cancer Prevention (PDQ®)—NCI (nciglobal,ncienterprise). (2023, October 15). [pdqCancerInfoSummary]. https://www.cancer.gov/types/uterine/hp/endometrial-prevention-pdq
Fan, X., Zou, X., Liu, C., Cheng, W., Zhang, S., Geng, X., & Zhu, W. (2021). MicroRNA expression profile in serum reveals novel diagnostic biomarkers for endometrial cancer. Bioscience reports, 41(6), BSR20210111. https://doi.org/10.1042/BSR20210111
Felix, A. S., Weissfeld, J. L., Stone, R. A., Bowser, R., Chivukula, M., Edwards, R. P., & Linkov, F. (2010). Factors associated with Type I and Type II endometrial cancer. Cancer causes & control : CCC, 21(11), 1851–1856. https://doi.org/10.1007/s10552-010-9612-8
Feng, Y., Wang, Z., Zhu, M., Li, S., Dong, S., Gong, L., Li, X., Zhang, S., Jia, T., Kong, X., Tian, J., & Sun, L. (2022). Single Nucleotide Polymorphisms of EXOC1, BCL2, CCAT2, and CARD8 Genes and Susceptibility to Cervical Cancer in the Northern Chinese Han Population. Frontiers in oncology, 12, 878529. https://doi.org/10.3389/fonc.2022.878529
Fernandes, A., Viveros-Carreño, D., Hoegl, J., Ávila, M., & Pareja, R. (2022). Human papillomavirus independent cervical cancer. International journal of gynecologic cancer, 32(1). https://doi.org/10.1136/ijgc-2021-003014
Galant, N., Krawczyk, P., Monist, M., Obara, A., Gajek, Ł., Grenda, A., Nicoś, M., Kalinka, E., & Milanowski, J. (2024). Molecular Classification of Endometrial Cancer and Its Impact on Therapy Selection. International journal of molecular sciences, 25(11), 5893. https://doi.org/10.3390/ijms25115893
Gebert, M., Jaśkiewicz, M., Moszyńska, A., Collawn, J. F., & Bartoszewski, R. (2020). The effects of single nucleotide polymorphisms in cancer RNAi therapies. Cancers, 12(11), 3119. https://doi.org/10.3390/cancers12113119
Goldberg, A. D., Allis, C. D., & Bernstein, E. (2007). Epigenetics: A landscape takes shape. Cell, 128(4), 635–638. https://doi.org/10.1016/j.cell.2007.02.006
Gu, X., Shen, H., Bai, W., Xiang, Z., Li, X., Zhang, R., Shi, F., Li, H., Zhu, G., & Guo, S. (2022). Endometrial cancer prognosis prediction using correlation models based on CDK family genes. Frontiers in genetics, 13, 1021600. https://doi.org/10.3389/fgene.2022.1021600
Guduri, M., Kolluru, S., Pasupulati, H., & Satyanarayana, P. (2024). A Comprehensive Review on PARP Inhibitors in Targeted Therapy for Cancers. Journal of international research in medical and pharmaceutical sciences, 19(2), 44–59. https://doi.org/10.56557/jirmeps/2024/v19i28811
Helwa, R., Gansmo, L. B., Bjørnslett, M., Halle, M. K., Werner, H. M. J., Romundstad, P., Hveem, K., Vatten, L., Dørum, A., Lønning, P. E., & Knappskog, S. (2021). Impact of MDM2 promoter SNP55 (rs2870820) on risk of endometrial and ovarian cancer. Biomarkers: biochemical indicators of exposure, response, and susceptibility to chemicals, 26(4), 302–308. https://doi.org/10.1080/1354750X.2021.1891291
Hewavisenti, R. V., Arena, J., Ahlenstiel, C. L., & Sasson, S. C. (2023). Human papillomavirus in the setting of immunodeficiency: Pathogenesis and the emergence of next-generation therapies to reduce the high associated cancer risk. Frontiers in immunology, 14. https://doi.org/10.3389/fimmu.2023.1112513
Ho, H. Y., Chung, K. S., Kan, C. M., & Wong, S. C. (2024). Liquid Biopsy in the Clinical Management of Cancers. International journal of molecular sciences, 25(16). https://doi.org/10.3390/ijms25168594
Hirschl, N., Leveque, W., Granitto, J., Sammarco, V., Fontillas, M., & Penson, R. T. (2024). PARP Inhibitors: Strategic Use and Optimal Management in Ovarian Cancer. Cancers, 16(5). https://doi.org/10.3390/cancers16050932
Hitchins, M. P., Alvarez, R., Zhou, L., Aguirre, F., Dámaso, E., Pineda, M., Capella, G., Wong, J.J.L., Yuan, X., Ryan, S.R., Sathe, D.S., Baxter, M.D., Cannon, T., Biswas, R., DeMarco, T., Grzelak, D., Hampel, H., & Pearlman, R. (2023). MLH1-methylated endometrial cancer under 60 years of age as the “sentinel” cancer in female carriers of high-risk constitutional MLH1 epimutation. Gynecologic oncology, 171, 129-140. https://doi.org/10.1016/j.ygyno.2023.02.017
Hu, J., Xu, Z., Ye, Z., Li, J., Hao, Z., & Wang, Y. (2023). The association between single nucleotide polymorphisms and ovarian cancer risk: A systematic review and network meta-analysis. Cancer medicine, 12(1), 541–556. https://doi.org/10.1002/cam4.4891
Hrytsay, I., Mazur, Y., Ferneza, S., Sulaieva, O., & Volodko, N. (2024). Implementation of Molecular Profiling in the Diagnosis and Treatment Planning of Patients With Advanced Ovarian Cancer. Proceedings of the shevchenko scientific society. Medical sciences, 73(1). https://doi.org/10.25040/ntsh2024.01.13
Hung, W.-C., Wu, T.-F., Ng, S.-C., Lee, Y., Shen, H.-P., Yang, S.-F., & Wang, P.-H. (2019). Involvement of endothelial nitric oxide synthase gene variants in the aggressiveness of uterine cervical cancer. Journal of cancer, 10(12), 2594–2600. https://doi.org/10.7150/jca.33192
Ignatov, A., & Ortmann, O. (2020). Endocrine Risk Factors of Endometrial Cancer: Polycystic Ovary Syndrome, Oral Contraceptives, Infertility, Tamoxifen. Cancers, 12(7), 1766. https://doi.org/10.3390/cancers12071766
Isbilen, E., Ulusal, H., Karaer, K., Kul, S., Yaman, D. M., Tepe, N. B., Kanbur, H. C., Tarakcioglu, M., & Ozyurt, A. B. (2020). VDR gene polymorphisms as a significant factor in unexplained infertility. Gene reports, 21, 100962. https://doi.org/10.1016/j.genrep.2020.100962
Kanaya, T., Kyo, S., Sakaguchi, J., Maida, Y., Nakamura, M., Takakura, M., Hashimoto, M., Mizumoto, Y., & Inoue, M. (2005). Association of mismatch repair deficiency with PTEN frameshift mutations in endometrial cancers and the precursors in a Japanese population. American journal of clinical pathology, 124(1), 89–96. https://doi.org/10.1309/PAACLG8DXDK0X2B1
Katagiri, R., Iwasaki, M., Abe, S. K., Islam, M. R., Rahman, M. S., Saito, E., Merritt, M.A., Choi, J.Y., Shin, A., Sawada, N., Tamakoshi, A., Koh, W.P., Sakata, R., Tsuji, I., Kim, J., Nagata, C., Park, S.K., Kweon, S.S., Shu, X.O., Gao, Y.T., Tsugane, S., Kimura, T., Yuan, J.M., Kanemura, S., Lu, Y., Sugawara, Y., Wada, K., Shin, M.H., Ahsan, H., Boffetta, P., Chia, K.S., Matsuo, K., Qiao, Y.L., Rothman, N., Zheng, W., Inoue, M., & Kang, D. (2023). Reproductive factors and endometrial cancer risk among women. JAMA network open, 6(9), e2332296-e2332296. https://doi.org/10.1001/jamanetworkopen.2023.32296
Kaur Jawanda, I., Soni, T., Kumari, S., & Prabha, V. (2024). Deciphering the potential of proteomic based biomarkers in women’s reproductive diseases: Empowering precision medicine in gynecology. Biomarkers, 29(1), 7–17. https://doi.org/10.1080/1354750X.2024.2308827
Keyvani, V., Mollazadeh, S., Riahi, E., Alsadat, R. M., Anvari, K., & Avan, A. (2024). Nanotechnological Advances in the Diagnosis of Gynecological Cancers and Nanotheranostics. Current pharmaceutical design, 30(33), 2619–2630. https://doi.org/10.2174/0113816128317605240628063731
Khatami, F., Shahriari, S., Aminimoghaddam, S., Klashami, Z. N., Farahani, M. S., Teimoori-Toolabi, L., Amoli, M.A., Asadi, M., & Rashidi, B. H. (2023). PTEN promoter methylation and expression in endometrial cancer tissues. Epigenomics, 15(8), 507-516. https://doi.org/10.2217/epi-2023-0099
Kiani, P., Vatankhahan, H., Zare-Hoseinabadi, A., Ferdosi, F., Ehtiati, S., Heidari, P., Dorostgou, Z., Movahedpour, Baktash, A., Rajabivahid, M., & Khatami, S. H. (2024). Electrochemical biosensors for early detection of breast cancer. Clinica chimica acta, 119923. https://doi.org/10.1016/j.cca.2024.119923
Kokilavani, R., Kotal, H., Kaushik, A., & Jana, Saikat K. (2024). Nanotechnology-Assisted Electrochemical Immunosensors for Human Reproductive Cancer Diagnostics: Toward Laboratory to Clinics to Personalized Health Care. Journal of the electrochemical society, 171(5), 057516. https://doi.org/10.1149/1945-7111/ad4c57
Kokemüller, L., Ramachandran, D., Schürmann, P., Geffers, R., Jentschke, M., Böhmer, G., Strauß, H.G., Hirchenhain, C., Schmidmayr, M., Müller, F., Fasching, P.A., Luyten, A., Häfner, N., Hillemanns, P., & Dörk, T. (2025). Germline variants of homology-directed repair or mismatch repair genes in cervical cancer. International journal of cancer. https://doi.org/10.1002/ijc.35221
Koo, K. H., Jeong, W. J., Cho, Y. H., Park, J. C., & Choi, K. Y. (2015). K-Ras stabilization by estrogen via PKCδ is involved in endometrial tumorigenesis. Oncotarget, 6(25), 21328. https://doi.org/10.18632/oncotarget.4049
Kotrikadze, N., Tufinashvili, T., Nakashidze, I., Ramishvili, L., Alibegashvili, M., Gordeziani, M., Sepiashvilli, B., & Ahmad, S. (2019a). Morpho-structural Peculiarities of Blood Formed Elements and Clinic-pathological Characteristics in Women with Uterine (Benign, Malignant) Tumors in Menopausal Age. The FASEB journal, 33(S1). https://doi.org/10.1096/fasebj.2019.33.1_ supplement.495.7
Kotrikadze, N., Tufinashvili, T., Ramishvili, L., Alibegashvili, M., Nakashidze, I., Gordeziani, M., Sepiashvilli, B., & Ahmad, S. (2019b). The study of the antioxidant enzymes, the activity of acid phosphatase and alteration of lipid peroxidation in women with uterine tumors. E-Poster Viewings, A108.3-A109. https://doi.org/10.1136/ijgc-2019-IGCS.255
Kotrikadze, N., Tupinashvili, T., Ramishvili, L., Alibegashvili, M., Nakashidze, I., Nemsadze, G., Gordeziani, M., Khazaradze, A., Sepiashvilli, B., & Ahmad, S. (2019c). Differential assessments of blood lipids, lipid peroxidation, antioxidant status, and fatty acids in women with uterine tumors during menopausal period. Gynecologic oncology, 154, 99–100. https://doi.org/10.1016/j.ygyno.2019.04.236
Kotrikadze, N., Alibegashvili, M., Ramishvili, L., Nakashidze, I., Tevdoradze, T., Gordeziani, M., Zibzibadze, M., Khazaradze, A., Sepiashvilli, B., & Ahmad, S. (2020). Thermodynamic parameters of blood plasma proteins in women with breast tumors. Gynecologic oncology, 159, 357. https://doi.org/10.1016/j.ygyno.2020.05.671
Kovarova, A., Kastrati, G., Pekarkova, J., Metelka, R., Drbohlavova, J., Bilkova, Z., Selesovska, R., & Korecka, L. (2023). Biosensor with electrochemically active nanocomposites for signal amplification and simultaneous detection of three ovarian cancer biomarkers. Electrochimica acta, 469, 143213. https://doi.org/10.1016/J.ELECTACTA.2023.143213
Kumar, G.G., Paul, S. F. D., Molia, C., Manickavasagam, M., Ramya, R., Usha Rani, G., Ganesan, N., & Andrea Mary, F. (2022). The association between CYP17A1, CYP19A1, and HSD17B1 gene polymorphisms of estrogen synthesis pathway and ovarian cancer predisposition. Meta gene, 31, 100985. https://doi.org/10.1016/j.mgene.2021.100985
Kumar, V. R., Kampan, N. C., Abd Aziz, N. H., Teik, C. K., Shafiee, M. N., & Menon, P. S. (2023). Recent Advances in Surface Plasmon Resonance (SPR) Technology for Detecting Ovarian Cancer Biomarkers. Cancers, 15(23), 1–26. https://doi.org/10.3390/cancers15235607
Kuntamung, K., Sangthong, P., Jakmunee, J., & Ounnunkad, K. (2024). Simultaneous immunodetection of multiple cervical cancer biomarkers based on a signal-amplifying redox probes/polyethyleneimine-coated gold nanoparticles/2D tungsten disulfide/graphene oxide nanocomposite platform. Bioelectrochemistry, 160, 108780. https://doi.org/10.1016/J.BIOELECHEM.2024.108780
Leitão, S. T., Rubiales, D., & Vaz Patto, M. C. (2023). Identification of novel sources of partial and incomplete hypersensitive resistance to rust and associated genomic regions in common bean. BMC plant biology, 23(1), 610. https://doi.org/10.1186/s12870-023-04619-8
Li, D., Liu, Y., Kong, D., Papukashvili, D., Rcheulishvili, N., Zhao, H., Li, Y., Hou, C., Ma, J., Lu, X., & Bai, W. (2022). Vitamin D Receptor Gene Polymorphisms and the Risk of CIN2+ in Shanxi Population. BioMed research international, 2022, 1–9. https://doi.org/10.1155/2022/6875996
Lim, D., & Oliva, E. (2010). Nonendometrioid endometrial carcinomas. Seminars in diagnostic pathology, 27(4), 241–260. https://doi.org/10.1053/j.semdp.2010.09.004
Liu, G.-C., Zhou, Y.-F., Su, X.-C., & Zhang, J. (2019). Interaction between TP53 and XRCC1 increases susceptibility to cervical cancer development: A case control study. BMC cancer, 19(1), 24. https://doi.org/10.1186/s12885-018-5149-0
Liu, H., Sun, L., Liu, X., Wang, R., & Luo, Q. (2023a). Associations between non-coding RNAs genetic polymorphisms with ovarian cancer risk: A systematic review and meta-analysis update with trial sequential analysis. Medicine, 102(39), e35257. https://doi.org/10.1097/MD.0000000000035257
Liu, L., Habeshian, T. S., Zhang, J., Peeri, N. C., Du, M., De Vivo, I., & Setiawan, V. W. (2023b). Differential trends in rising endometrial cancer incidence by age, race, and ethnicity. JNCI cancer spectrum, 7(1), pkad001. https://doi.org/10.1093/jncics/pkad001
Lm, D., Rj, W., Ua, A., Sd, S., & Cr, E. (2011). Trends in endometrial cancer incidence rates in the United States, 1999-2006. Journal of women’s health (2002), 20(8). https://doi.org/10.1089/jwh.2010.2529
Mahdy, H., Casey, M. J., & Crotzer, D. (2022). Endometrial Cancer. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK525981/
Makker, V., MacKay, H., Ray-Coquard, I., Levine, D. A., Westin, S. N., Aoki, D., & Oaknin, A. (2021). Endometrial cancer. Nature reviews disease primers, 7(1), 88. https://doi.org/10.1038/s41572021-00324-8
Malonek, D., Dekel, B. Z., Haran, G., Reens-Carmel, R., Groisman, G. M., Hallak, M., & Bruchim, I. (2020). Rapid intraoperative diagnosis of gynecological cancer by ATR-FTIR spectroscopy of fresh tissue biopsy. Journal of biophotonics, 13(9), 1–10. https://doi.org/10.1002/jbio.202000114
Marković, A., Grujičić, D., Živković Radojević, M., & Milošević-Djordjević, O. (2024). Measurement of chromosomal instability and level of DNA damage in peripheral blood mononuclear cells of endometrial cancer patients. Mutagenesis, 39(3), 172-180. https://doi.org/10.1093/mutage/ geae003
McInerney, E. M., & Katzenellenbogen, B. S. (1996). Different regions in activation function-1 of the human estrogen receptor required for antiestrogen- and estradiol-dependent transcription activation. The journal of biological chemistry, 271(39), 24172–24178. https://doi.org/10.1074/jbc.271.39.24172
Metzger, D., Ali, S., Bornert, J.-M., & Chambon, P. (1995). Characterization of the Amino-terminal Transcriptional Activation Function of the Human Estrogen Receptor in Animal and Yeast Cells. Journal of biological chemistry, 270(16), 9535–9542. https://doi.org/10.1074/jbc.270.16.9535
Miyamoto, T., Shiozawa, T., Kashima, H., Feng, Y.-Z., Suzuki, A., Kurai, M., Nikaido, T., & Konishi, I. (2006). Estrogen up-regulates mismatch repair activity in normal and malignant endometrial glandular cells. Endocrinology, 147(10), 4863–4870. https://doi.org/10.1210/en.2006-0632
Momenimovahed, Z., Tiznobaik, A., Taheri, S., & Salehiniya, H. (2019). Ovarian cancer in the world: Epidemiology and risk factors. International journal of women’s health, 11, 287–299. https://doi.org/10.2147/IJWH.S197604
Moreno-Bueno, G., Rodríguez-Perales, S., Sánchez-Estévez, C., Hardisson, D., Sarrió, D., Prat, J., Cigudosa, J. C., Matias-Guiu, X., & Palacios, J. (2003). Cyclin D1 gene (CCND1) mutations in endometrial cancer. Oncogene, 22(38), 6115–6118. https://doi.org/10.1038/sj.onc.1206868
Nakashidze, I., & Ahmad, S. (2019). Genetic predisposition for pancreatic cancer. In Theranostic Approach for Pancreatic Cancer (pp. 153–169). Elsevier. https://doi.org/10.1016/B978-0-12819457-7.00008-6
Nakashidze, I., Dariya, B., Peshkova, T., & Beridze, S. (2020). The Genetic Polymorphisms in Colon Cancer. Critical reviewsTM in oncogenesis, 25(4), 405–415. https://doi.org/10.1615/CritRevOncog.2020035957
Nakashidze, I., Diasamidze, A., Baratashvili, D., Nagervadze, M., Alibegashvili, M., Ramishvili, L., Gordeziani, M., Khazaradze, A., & Kotrikadze, N. (2014). Alteration of Sex and Non-Sex Hormones and Distribution Features of Blood ABO System Groups among the Women with Uterine Body
Tumors. Journal of cancer therapy, 05(05), 411–419. https://doi.org/10.4236/jct.2014.55047
Nees, L. K., Heublein, S., Steinmacher, S., Juhasz-Böss, I., Brucker, S., Tempfer, C. B., & Wallwiener, M. (2022). Endometrial hyperplasia as a risk factor of endometrial cancer. Archives of gynecology and obstetrics, 1-15. https://doi.org/10.1007/s00404-021-06380-5
Nujhat, S., Leese, H. S., Di Lorenzo, M., Bowen, R., & Moise, S. (2023). Advances in screening and diagnostic lab-on-chip tools for gynaecological cancers–a review. Artificial cells, nanomedicine and biotechnology, 51(1), 618–629. https://doi.org/10.1080/21691401.2023.2274047
Ouh, Y. T., Oh, Y., Joo, J., Woo, J. H., Han, H. J., Cho, H. W., Lee, J.K., Chun, Y., Lim, M.N., & Hong, J. H. (2024). Assessing the New 2020 ESGO/ESTRO/ESP Endometrial Cancer Risk Molecular Categorization System for Predicting Survival and Recurrence. Cancers, 16(5), 965. https://doi.org/10.3390/cancers16050965
Ozgor, B. Y., Iyibozkurt, C., Bastu, E., Berkman, S., Yalcın, O., Cakmakoglu, B., & Saygılı, H. (2019). Investigation of resistin 420 and 62 gene polymorphism in patients with endometrial cancer. Taiwanese journal of obstetrics & gynecology, 58(1), 164–167. https://doi.org/10.1016/j.tjog.2018.11.030
Park, J. E., Lee, T., Cho, E. H., Jang, M. A., Won, D., Park, B., Ki, C.S., & Kong, S. Y. (2024). Carrier Frequency and Incidence of MUTYH-Associated Polyposis Based on Database Analysis in East Asians and Koreans. Annals of laboratory medicine, 45(1), 77. https://doi.org/10.3343/alm.2024.0242
Parvez, A., Choudhary, F., Mudgal, P., Khan, R., Qureshi, K. A., Farooqi, H., & Aspatwar, A. (2023). PD-1 and PD-L1: Architects of immune symphony and immunotherapy breakthroughs in cancer treatment. Frontiers in immunology, 14, 1–16. https://doi.org/10.3389/fimmu.2023.1296341
Pandya, D., Tomita, S., Rhenals, M. P., Swierczek, S., Reid, K., Camacho-Vanegas, O., Camacho, C., Engelman, K., Polukort, S., RoseFigura, J., Chuang, L., Andikyan, V., Cohen, S., Fiedler, P., Sieber, S., Shih, I.M., Billaud, J.N., Sebra, R., Reva, B., Dottino, P., & Martignetti, J. A. (2024). Mutations in cancer-relevant genes are ubiquitous in histologically normal endometrial tissue. Gynecologic oncology, 185, 194-201. https://doi.org/10.1016/j.ygyno.2024.02.027
Pati, S., Irfan, W., Jameel, A., Ahmed, S., & Shahid, R. K. (2023). Obesity and cancer: a current overview of epidemiology, pathogenesis, outcomes, and management. Cancers, 15(2), 485. https://doi.org/10.3390/cancers15020485
Petrović, N., Nakashidze, I. & Nedeljković, M. Breast Cancer Response to Therapy: Can microRNAs Lead the Way?. J Mammary Gland Biol Neoplasia 26, 157–178 (2021). https://doi.org/10.1007/s10911-021-09478-3
Petrovic, N., Sami, A., Martinovic, J., Zaric, M., Nakashidze, I., Lukic, S., & Jovanovic-Cupic, S. (2017). TIMP-3 mRNA expression levels positively correlates with levels of miR-21 in in situ BC and negatively in PR positive invasive BC. Pathology - research and practice, 213(10), 1264-1270. https://doi.org/10.1016/j.prp.2017.08.012
Pierre, M. D., Edy, M., Fletcher Prieto, M. D., Viviana, A., Hernández Blanquisett MD, A., Gómez Camacho, M. D., Medina, R.P., Silva, L.M., Fernández, R., & desarrollador del Consenso, G. (2024). Colombian consensus for the molecular diagnosis of endometrial cancer. Revista
colombiana de obstetricia y ginecología, 75(1). https://doi.org/10.18597/rcog.4060
Prakash, A., Das Purkayastha, B. P., Srivastava, S., Chaturvedi, S., Ali, A., Aggarwal, D. D., & Roy, J. K. (2022). Novel Variant Identified in the Enhancer Region of Host Transcription Factor, BRN3A, is a Significant Risk Factor for HPV-Induced Uterine Cervix Cancer. International journal of molecular and cellular medicine, 11(2), 88–103. https://doi.org/10.22088/IJMCM.BUMS.11.2.88
Priya, N. D., Kumar, K. V. N., Charani, M. S., Bindu, D., Reddy, K. L., & Gowthami, Y. (2024). Biomarker Panel for Early Detection in Uterine Cancer: A Review. Asia pacific journal of cancer biology, 9(2), 201–208. https://doi.org/10.31557/APJCB.2024.9.2.201
Rahman, M. A., Hasan, M. M., Hossain, A., Alam, K. M., Sultana, R., Mazid, M. A., & Rahman, M. M. (2023). Analysis of E-cadherin (CDH1) Gene Polymorphism and Its Association with Cervical Cancer Risk in Bangladeshi Women. Asian pacific journal of cancer prevention: APJCP, 24(7), 2361–2368. https://doi.org/10.31557/APJCP.2023.24.7.2361
Rahmani, F., Hasanzadeh, M., Hassanian, S. M., Khazaei, M., Esmaily, H., Asef-Agah, S. A., Naghipour, A., A Ferns, G., & Avan, A. (2020). Association of a genetic variant in the angiopoietin like protein 4 gene with cervical cancer. Pathology, research and practice, 216(7), 153011. https://doi.org/10.1016/j.prp.2020.153011
Rodriguez, A. C., Blanchard, Z., Maurer, K. A., & Gertz, J. (2019). Estrogen signaling in endometrial cancer: a key oncogenic pathway with several open questions. Hormones and cancer, 10, 51-63. https://doi.org/10.1007/s12672-019-0358-9
Rockett, T. W., Almahyawi, M., Ghimire, M. L., Jonnalagadda, A., Tagliaferro, V., Seashols-Williams, S. J., Bertino, M. F., Caputo, G. A., & Reiner, J. E. (2024). Cluster-Enhanced Nanopore Sensing of Ovarian Cancer Marker Peptides in Urine. ACS sensors, 9(2), 860–869. https://doi.org/10.1021/acssensors.3c02207
Ruiz De La Cruz, M., De La Cruz Montoya, A. H., Rojas Jiménez, E. A., Martínez Gregorio, H., Díaz Velásquez, C. E., Paredes De La Vega, J., De La Cruz Hernández-Hernández, F., & Vaca Paniagua, F. (2021). Cis-Acting Factors Causing Secondary Epimutations: Impact on the Risk for
Cancer and Other Diseases. Cancers, 13(19), 4807. https://doi.org/10.3390/cancers13194807
Saegusa, M., Hashimura, M., Yoshida, T., & Okayasu, I. (2001). β-Catenin mutations and aberrant nuclear expression during endometrial tumorigenesis. British journal of cancer, 84(2), 209–217. https://doi.org/10.1054/bjoc.2000.1581
Sahin, S., & Yıldırım Tirgil, N. (2024). Circulating tumor DNA (ctDNA) Detection via electrochemical Biosensing Tools. MANAS journal of engineering, 12(1), 104–115. https://doi.org/10.51354/mjen.1375211
Shahazi, R., Saddam, A. I., Islam, M. R., Rahman, M. M., Paimard, G., Kumer, A., Alam, Md. M., & Mahamud, Md. K. (2024). Recent progress in Nanomaterial based biosensors for the detection of cancer biomarkers in human fluids. Nano carbons, 2(2), 1254. https://doi.org/10.59400/n-c.v2i2.1254
Shaikh, A. P., Khurana, R., Shaikh, N. P., Barua, J. D., Ali, A., Murvanidze, I., Saralidze, E., & Nakashidze, I. (2023). Peculiarities of some candidate gene polymorphisms in Parkinson’s disease. Pomeranian journal of life sciences, 69(2), Article 2. https://doi.org/10.21164/pomjlifesci.893
Shaikh, A. P., Shaikh, N. P., & Irina, N. (2022). VDR Gene SNPs in Gastrointestinal Tumors. JSM gastroenterology and hepatology. https://doi.org/10.47739/2373-9487/1111
Shaikh, N. P., Murvanidze, I., Shaikh, A. P., Khurana, R., & Nakashidze, I. (2023). The Altered Gene Expression and Epigenetic Mechanisms in Breast Cancer. Journal of biomedical research & environmental sciences, 4(10), 1461–1469. https://doi.org/10.37871/jbres1819
Sherman, M. E., Sturgeon, S., Brinton, L. A., Potischman, N., Kurman, R. J., Berman, M. L., Mortel, R., Twiggs, L. B., Barrett, R. J., & Wilbanks, G. D. (1997). Risk factors and hormone levels in patients with serous and endometrioid uterine carcinomas. Modern pathology: An official journal of the united states and canadian academy of pathology, Inc, 10(10), 963–968.
Sofiyeva, N., Krakstad, C., Halle, M. K., O’Mara, T. A., Romundstad, P., Hveem, K., Vatten, L., Lønning, P. E., Gansmo, L. B., & Knappskog, S. (2023). APOBEC3A/B deletion polymorphism and endometrial cancer risk. Cancer medicine, 12(6), 6659–6667. https://doi.org/10.1002/cam4.5448
Srinivasan, S., Clements, J. A., & Batra, J. (2016). Single nucleotide polymorphisms in clinics: Fantasy or reality for cancer?. Critical reviews in clinical laboratory sciences, 53(1), 29-39. https://doi.org/10.3109/10408363.2015.1075469
Vitamin D receptor gene polymorphisms and uterine fibroid incidence in Caucasian women. (n.d.). Retrieved December 8, 2023, from https://www.archivesofmedicalscience.com/Vitamin-D receptor-gene-polymorphisms-and-uterine-fibroid-incidence-in-Caucasian,99548,0,2.html
Vegesna, Dr. V. (2024). AI-Driven Personalized Medicine: A Frame Work for Tailored Cancer Treatment. International journal of innovative research in advanced engineering, 11(06), 747-752. https://doi.org/10.26562/ijirae.2024.v1106.06
Wakkerman, F. C., Wu, J., Putter, H., Jürgenliemk-Schulz, I. M., Jobsen, J. J., Lutgens, L. C., Haverkort, M.A.D., de Jong, M.A., Mens, J.W.M., Wortman, B.G., Nout, R.A., Léon-Castillo, A., Powell, M.E., Mileshkin, L.R., Katsaros, D., Alfieri, J., Leary, A., Singh, N., de Boer, S.M., Nijman, H.W., Smit, V.T.H.B.M., Bosse, T., Koelzer, V.H., Creutzberg, C.L., & Horeweg, N. (2024). Prognostic impact and causality of age on oncological outcomes in women with endometrial cancer: a multimethod analysis of the randomised PORTEC-1, PORTEC-2, and PORTEC-3 trials. The lancet oncology, 25(6), 779-789. https://doi.org/10.1016/S1470-2045(24)00142-6
Wang, S., Sun, H., Jia, Y., Tang, F., Zhou, H., Li, X., Zhou, J., Huang, K., Zhang, Q., Hu, T., Yang, R., Wang, C., Xi, L., Deng, D., Wang, H., Wang, S., Ma, D., & Li, S. (2015). Association of 42 SNPs with genetic risk for cervical cancer: An extensive meta-analysis. BMC medical genetics, 16(1), 25. https://doi.org/10.1186/s12881-015-0168-z
Wang, H., Zhang, Y., Zhang, H., Cao, H., Mao, J., Chen, X., Wang, L., Zhang, N., Luo, P., Xue, J., Qi, X., Dong, X., Liu, G., & Cheng, Q. (2024). Liquid biopsy for human cancer: Cancer screening, monitoring, and treatment. MedComm, 5(6), 1–24. https://doi.org/10.1002/mco2.564
Wang, X., Wang, L., Lin, H., Zhu, Y., Huang, D., Lai, M., Xi, X., Huang, J., Zhang, W., & Zhong, T. (2024). Research progress of CTC, ctDNA, and EVs in cancer liquid biopsy. Frontiers in oncology, 14, 1–22. https://doi.org/10.3389/fonc.2024.1303335
Wang, X., Glubb, D. M., & O’Mara, T. A. (2023). Dietary factors and endometrial cancer risk: a mendelian randomization study. Nutrients, 15(3), 603. https://doi.org/10.3390/nu15030603
Weisenberger, D. J., Siegmund, K. D., Campan, M., Young, J., Long, T. I., Faasse, M. A., Kang, G. H., Widschwendter, M., Weener, D., Buchanan, D., Koh, H., Simms, L., Barker, M., Leggett, B., Levine, J., Kim, M., French, A. J., Thibodeau, S. N., Jass, J., Haile, R., & Laird, P. W. (2006). CpG
island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nature genetics, 38(7), 787–793. https://doi.org/10.1038/ng1834
Williams, L., Henry, C., Simcock, B., & Filoche, S. (2024). Increasing incidence of endometrial cancer in Aotearoa New Zealand: Health professionals’ perspective. Australian and new zealand journal of obstetrics and gynaecology, 64, 114-119. https://doi.org/10.1111/ajo.13751
Wu, F., Gao, H., Qiu, R., Zhang, H., Ren, X., Qi, X., Miao, M., & Rui, C. (2024). A novel ratiometric electrochemical immunosensor for the detection of cancer antigen 125 based on three-dimensional carbon nanomaterial and MOFs. Microchemical journal, 200, 110372. https://doi.org/10.1016/J.MICROC.2024.110372
Xiong, X. D., Luo, X. P., Cheng, J., Liu, X., Li, E. M., & Zeng, L. Q. (2014). A genetic variant in pre-miR 27a is associated with a reduced cervical cancer risk in southern Chinese women. Gynecologic oncology, 132(2), 450-454. https://doi.org/10.1016/j.ygyno.2013.12.030
Xu, L., Qiu, Y., Feng, L., Zhou, L., Chen, X., & Yu, D. (2020). Correlation between single nucleotide polymorphisms of DACH1 gene microRNA binding site and susceptibility of patients with endometrial cancer. Medicine, 99(25), e20793. https://doi.org/10.1097/MD.0000000000020793
Yang, H. P., Wentzensen, N., Trabert, B., Gierach, G. L., Felix, A. S., Gunter, M. J., Hollenbeck, A., Park, Y., Sherman, M. E., & Brinton, L. A. (2013). Endometrial Cancer Risk Factors by 2 Main Histologic Subtypes. American journal of epidemiology, 177(2), 142–151. https://doi.org/10.1093/aje/kws200
Yi, T.-Z., Guo, J., Zhou, L., Chen, X., Mi, R.-R., Qu, Q.-X., Zheng, J.-H., & Zhai, L. (2011). Prognostic value of E-cadherin expression and CDH1 promoter methylation in patients with endometrial carcinoma. Cancer investigation, 29(1), 86–92. https://doi.org/10.3109/07357907.2010.512603
Yang, Y., Wu, S. F., & Bao, W. (2024). Molecular subtypes of endometrial cancer: Implications for adjuvant treatment strategies. International journal of gynecology & obstetrics, 164(2), 436-459. https://doi.org/10.1002/ijgo.14969
Zhang, Q.-Y., Yi, D.-Q., Zhou, L., Zhang, D.-H., & Zhou, T.-M. (2011). Status and significance of CpG island methylator phenotype in endometrial cancer. Gynecologic and obstetric investigation, 72(3), 183–191. https://doi.org/10.1159/000324496
Zhang, C., Li, T., Zhao, Q., Ma, R., Hong, Z., Huang, X., Gao, P., Liu, J., Zhao, J., & Wang, Z. (2024). Advances and Prospects in Liquid Biopsy Techniques for Malignant Tumor Diagnosis and Surveillance. Small, 2404709(77). https://doi.org/10.1002/smll.202404709
Zhang, R., Y Siu, M. K., S Ngan, H. Y., & L Chan, K. K. (2022). Molecular Biomarkers for the Early Detection of Ovarian Cancer. International journal of molecular sciences, 23(19), 12041. https://doi.org/10.3390/ijms231912041
Zmarzły, N., Januszyk, S., Mieszczański, P., Morawiec, E., Buda, P., Dziobek, K., Opławski, M., & Boroń, D. (2023). Endothelin-3 is epigenetically silenced in endometrioid endometrial cancer. Journal of cancer research and clinical oncology, 149(9), 5687-5696. https://doi.org/10.1007/s00432-02204525-w
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Nameera Parveen Shaikh, Joy Dip Barua, Aleena Parveen Shaikh, Sakshi Adhav, Nina Petrovic, Ermira Jahja, Tamar Peshkova, Irina Nakashidze

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.