The predictive value of metabolomic-related biomarkers in breast cancers: Current approaches in biotechnology
DOI:
https://doi.org/10.62063/rev-22Keywords:
AI, Biotechnology, Lipids, Metabolomics, Breast CancerAbstract
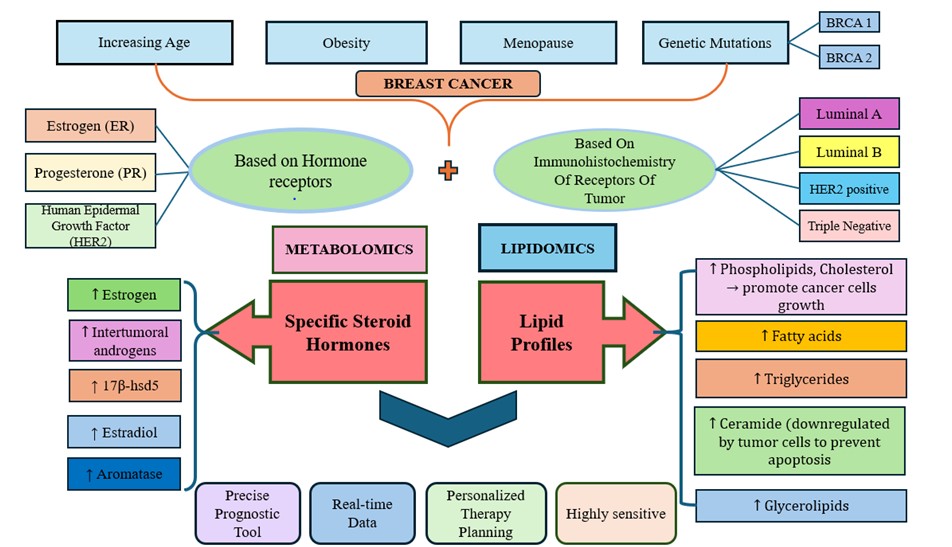
Breast cancer is the second most common cancer worldwide and is a leading cause of cancer-related mortality in women. The rising burden of breast cancer highlights the need for more accurate, non-invasive, and informative diagnostic tools. Despite the current advancements in medicine, predicting treatment response and patient prognosis remains challenging. It has thus become imperative to address the need for precise and reliable prognostic and diagnostic tools. Metabolic profiles, such as lipid processing and steroid hormone metabolism, have recently emerged as significant biomarkers in tumor biology, especially for early detection, prognosis, and therapy monitoring. This literature review explores the predictive value of serum lipid profiles and selected steroids as biomarkers in breast tumors. It shows their potential in improving diagnostic strategies and treatment planning in breast cancer management. These approaches offer valuable insights into tumor biology, metabolic changes, and hormone-driven pathways. Despite current challenges in sample preparation, data interpretation, and technical demands, recent advances such as high-resolution mass spectrometry, as well as spatial metabolomics and artificial intelligence, are helping to overcome these barriers. With continued research and technological progress, metabolomic-related biomarkers are expected to see broader use in clinical settings, supporting personalized treatment and improving outcomes for breast cancer patients.
References
Africander, D., & Storbeck, K.-H. (2018). Steroid metabolism in breast cancer: Where are we and what are we missing? Molecular and Cellular Endocrinology, 466, 86–97. https://doi.org/10.1016/j.mce.2017.05.016 DOI: https://doi.org/10.1016/j.mce.2017.05.016
Ahluwalia, K., Ebright, B., Chow, K., Dave, P., Mead, A., Poblete, R., Louie, S. G., & Asante, I. (2022). Lipidomics in Understanding Pathophysiology and Pharmacologic Effects in Inflammatory Diseases: Considerations for Drug Development. Metabolites, 12(4), 333. https://doi.org/10.3390/metabo12040333 DOI: https://doi.org/10.3390/metabo12040333
Anh, N. H., Long, N. P., Kim, S. J., Min, J. E., Yoon, S. J., Kim, H. M., Yang, E., Hwang, E. S., Park, J. H., Hong, S.-S., & Kwon, S. W. (2019). Steroidomics for the Prevention, Assessment, and Management of Cancers: A Systematic Review and Functional Analysis. Metabolites, 9(10), 199. https://doi.org/10.3390/metabo9100199 DOI: https://doi.org/10.3390/metabo9100199
Anh, N. K., Thu, N. Q., Tien, N. T. N., Long, N. P., & Nguyen, H. T. (2024). Advancements in Mass Spectrometry-Based Targeted Metabolomics and Lipidomics: Implications for Clinical Research. Molecules, 29(24), 5934. https://doi.org/10.3390/molecules29245934 DOI: https://doi.org/10.3390/molecules29245934
Babiker, F. (2002). Estrogenic hormone action in the heart: Regulatory network and function. Cardiovascular Research, 53(3), 709–719. https://doi.org/10.1016/S0008-6363(01)00526-0 DOI: https://doi.org/10.1016/S0008-6363(01)00526-0
Bathen, T. F., Geurts, B., Sitter, B., Fjøsne, H. E., Lundgren, S., Buydens, L. M., Gribbestad, I. S., Postma, G., & Giskeødegård, G. F. (2013). Feasibility of MR Metabolomics for Immediate Analysis of Resection Margins during Breast Cancer Surgery. PLoS ONE, 8(4), e61578. https://doi.org/10.1371/journal.pone.0061578 DOI: https://doi.org/10.1371/journal.pone.0061578
Caceres, S., Peña, L., Silvan, G., Illera, M. J., Woodward, W. A., Reuben, J. M., & Illera, J. C. (2016). Steroid Tumor Environment in Male and Female Mice Model of Canine and Human Inflammatory Breast Cancer. BioMed Research International, 2016, 1–7. https://doi.org/10.1155/2016/8909878 DOI: https://doi.org/10.1155/2016/8909878
Cao, Y., Xia, B., Zhang, Z., Hu, D., Huang, X., Yuan, J., & Li, F. (2023). Association of Body Fat Distribution and Risk of Breast Cancer in Pre- and Postmenopausal Women. Obesity Facts, 16(4), 356–363. https://doi.org/10.1159/000529834 DOI: https://doi.org/10.1159/000529834
Capper, C. P., Rae, J. M., & Auchus, R. J. (2016). The Metabolism, Analysis, and Targeting of Steroid Hormones in Breast and Prostate Cancer. Hormones and Cancer, 7(3), 149–164. https://doi.org/10.1007/s12672-016-0259-0 DOI: https://doi.org/10.1007/s12672-016-0259-0
Carmona, A., Mitri, S., James, T. A., & Ubellacker, J. M. (2024). Lipidomics and metabolomics as potential biomarkers for breast cancer progression. Npj Metabolic Health and Disease, 2(1), 24. https://doi.org/10.1038/s44324-024-00027-0 DOI: https://doi.org/10.1038/s44324-024-00027-0
Chen, X., Chen, H., Dai, M., Ai, J., Li, Y., Mahon, B., Dai, S., & Deng, Y. (2016). Plasma lipidomics profiling identified lipid biomarkers in distinguishing early-stage breast cancer from benign lesions. Oncotarget, 7(24), 36622–36631. https://doi.org/10.18632/oncotarget.9124 DOI: https://doi.org/10.18632/oncotarget.9124
Chou, F.-J., Liu, Y., Lang, F., & Yang, C. (2021). D-2-Hydroxyglutarate in Glioma Biology. Cells, 10(9), 2345. https://doi.org/10.3390/cells10092345 DOI: https://doi.org/10.3390/cells10092345
Clish, C. B. (2015). Metabolomics: An emerging but powerful tool for precision medicine. Molecular Case Studies, 1(1), a000588. https://doi.org/10.1101/mcs.a000588 DOI: https://doi.org/10.1101/mcs.a000588
Colomer, R., González-Farré, B., Ballesteros, A. I., Peg, V., Bermejo, B., Pérez-Mies, B., De La Cruz, S., Rojo, F., Pernas, S., & Palacios, J. (2024). Biomarkers in breast cancer 2024: An updated consensus statement by the Spanish Society of Medical Oncology and the Spanish Society of Pathology. Clinical and Translational Oncology, 26(12), 2935–2951. https://doi.org/10.1007/s12094-024-03541-1 DOI: https://doi.org/10.1007/s12094-024-03541-1
Criscitiello, C., & Corti, C. (2022). Breast Cancer Genetics: Diagnostics and Treatment. Genes, 13(9), 1593. https://doi.org/10.3390/genes13091593 DOI: https://doi.org/10.3390/genes13091593
Familial breast cancer: Collaborative reanalysis of individual data from 52 epidemiological studies including 58 209 women with breast cancer and 101 986 women without the disease. (2001). The Lancet, 358(9291), 1389–1399. https://doi.org/10.1016/S0140-6736(01)06524-2 DOI: https://doi.org/10.1016/S0140-6736(01)06524-2
Fang, Z., Ren, G., Ke, S., Xu, Q., Chen, Y., Shi, X., Guo, C., & Huang, J. (2025). Serum metabolomic profiling for predicting therapeutic response and toxicity in breast cancer neoadjuvant chemotherapy: A retrospective longitudinal study. Breast Cancer Research, 27(1), 2. https://doi.org/10.1186/s13058-024-01956-w DOI: https://doi.org/10.1186/s13058-024-01956-w
Freudenheim, J. L. (2020). Alcohol's Effects on Breast Cancer in Women. Alcohol Research: Current Reviews, 40(2), arcr.v40.2.11. https://doi.org/10.35946/arcr.v40.2.11 DOI: https://doi.org/10.35946/arcr.v40.2.11
Fu, Y., Zou, T., Shen, X., Nelson, P. J., Li, J., Wu, C., Yang, J., Zheng, Y., Bruns, C., Zhao, Y., Qin, L., & Dong, Q. (2021). Lipid metabolism in cancer progression and therapeutic strategies. MedComm, 2(1), 27–59. https://doi.org/10.1002/mco2.27 DOI: https://doi.org/10.1002/mco2.27
Ghini, V., Laera, L., Fantechi, B., Del Monte, F., Benelli, M., McCartney, A., Tenori, L., Luchinat, C., & Pozzessere, D. (2020). Metabolomics to Assess Response to Immune Checkpoint Inhibitors in Patients with Non-Small-Cell Lung Cancer. Cancers, 12(12), 3574. https://doi.org/10.3390/cancers12123574 DOI: https://doi.org/10.3390/cancers12123574
Giaquinto, A. N., Sung, H., Miller, K. D., Kramer, J. L., Newman, L. A., Minihan, A., Jemal, A., & Siegel, R. L. (2022). Breast Cancer Statistics, 2022. CA: A Cancer Journal for Clinicians, 72(6), 524–541. https://doi.org/10.3322/caac.21754 DOI: https://doi.org/10.3322/caac.21754
Griffin, J. L., & Shockcor, J. P. (2004). Metabolic profiles of cancer cells. Nature Reviews Cancer, 4(7), 551–561. https://doi.org/10.1038/nrc1390 DOI: https://doi.org/10.1038/nrc1390
Haddad, T. C., & Goetz, M. P. (2015). Landscape of Neoadjuvant Therapy for Breast Cancer. Annals of Surgical Oncology, 22(5), 1408–1415. https://doi.org/10.1245/s10434-015-4405-7 DOI: https://doi.org/10.1245/s10434-015-4405-7
Hammes, S. R., & Levin, E. R. (2019). Impact of estrogens in males and androgens in females. Journal of Clinical Investigation, 129(5), 1818–1826. https://doi.org/10.1172/JCI125755 DOI: https://doi.org/10.1172/JCI125755
He, Z., Chen, Z., Tan, M., Elingarami, S., Liu, Y., Li, T., Deng, Y., He, N., Li, S., Fu, J., & Li, W. (2020). A review on methods for diagnosis of breast cancer cells and tissues. Cell Proliferation, 53(7), e12822. https://doi.org/10.1111/cpr.12822 DOI: https://doi.org/10.1111/cpr.12822
Hickey, T. E., Robinson, J. L. L., Carroll, J. S., & Tilley, W. D. (2012). Minireview: The Androgen Receptor in Breast Tissues: Growth Inhibitor, Tumor Suppressor, Oncogene? Molecular Endocrinology, 26(8), 1252–1267. https://doi.org/10.1210/me.2012-1107 DOI: https://doi.org/10.1210/me.2012-1107
Hilvo, M., Denkert, C., Lehtinen, L., Müller, B., Brockmöller, S., Seppänen-Laakso, T., Budczies, J., Bucher, E., Yetukuri, L., Castillo, S., Berg, E., Nygren, H., Sysi-Aho, M., Griffin, J. L., Fiehn, O., Loibl, S., Richter-Ehrenstein, C., Radke, C., Hyötyläinen, T., … Orešič, M. (2011). Novel Theranostic Opportunities Offered by Characterization of Altered Membrane Lipid Metabolism in Breast Cancer Progression. Cancer Research, 71(9), 3236–3245. https://doi.org/10.1158/0008-5472.CAN-10-3894 DOI: https://doi.org/10.1158/0008-5472.CAN-10-3894
Hong, B. V., Rhodes, C. H., Agus, J. K., Tang, X., Zhu, C., Zheng, J. J., & Zivkovic, A. M. (2023). A single 36-h water-only fast vastly remodels the plasma lipidome. Frontiers in Cardiovascular Medicine, 10, 1251122. https://doi.org/10.3389/fcvm.2023.1251122 DOI: https://doi.org/10.3389/fcvm.2023.1251122
Horn, A., & Jaiswal, J. K. (2019). Structural and signaling role of lipids in plasma membrane repair. In Current Topics in Membranes (Vol. 84, pp. 67–98). Elsevier. https://doi.org/10.1016/bs.ctm.2019.07.001 DOI: https://doi.org/10.1016/bs.ctm.2019.07.001
Iacopetta, D., Rechoum, Y., & Fuqua, S. A. W. (2012). The role of androgen receptor in breast cancer. Drug Discovery Today: Disease Mechanisms, 9(1–2), e19–e27. https://doi.org/10.1016/j.ddmec.2012.11.003 DOI: https://doi.org/10.1016/j.ddmec.2012.11.003
Idle, J. R., & Gonzalez, F. J. (2007). Metabolomics. Cell Metabolism, 6(5), 348–351. https://doi.org/10.1016/j.cmet.2007.10.005 DOI: https://doi.org/10.1016/j.cmet.2007.10.005
Imai, Y., Youn, M., Kondoh, S., Nakamura, T., Kouzmenko, A., Matsumoto, T., Takada, I., Takaoka, K., & Kato, S. (2009). Estrogens Maintain Bone Mass by Regulating Expression of Genes Controlling Function and Life Span in Mature Osteoclasts. Annals of the New York Academy of Sciences, 1173(s1). https://doi.org/10.1111/j.1749-6632.2009.04954.x DOI: https://doi.org/10.1111/j.1749-6632.2009.04954.x
Iqbal, M. A., Siddiqui, S., Smith, K., Singh, P., Kumar, B., Chouaib, S., & Chandrasekaran, S. (2023). Metabolic stratification of human breast tumors reveal subtypes of clinical and therapeutic relevance. iScience, 26(10), 108059. https://doi.org/10.1016/j.isci.2023.108059 DOI: https://doi.org/10.1016/j.isci.2023.108059
Irzaldy, A., Gvamichava, R., Beruchashvili, T., Sturua, L., Van Ravesteyn, N. T., De Koning, H. J., & Heijnsdijk, E. A. M. (2024). Breast Cancer Screening in Georgia: Choosing the Most Optimal and Cost-Effective Strategy. Value in Health Regional Issues, 39, 66–73. https://doi.org/10.1016/j.vhri.2023.09.002 DOI: https://doi.org/10.1016/j.vhri.2023.09.002
Jafari, S. H., Saadatpour, Z., Salmaninejad, A., Momeni, F., Mokhtari, M., Nahand, J. S., Rahmati, M., Mirzaei, H., & Kianmehr, M. (2018). Breast cancer diagnosis: Imaging techniques and biochemical markers. Journal of Cellular Physiology, 233(7), 5200–5213. https://doi.org/10.1002/jcp.26379 DOI: https://doi.org/10.1002/jcp.26379
Ji, H., Hu, C., Yang, X., Liu, Y., Ji, G., Ge, S., Wang, X., & Wang, M. (2023). Lymph node metastasis in cancer progression: Molecular mechanisms, clinical significance and therapeutic interventions. Signal Transduction and Targeted Therapy, 8(1), 367. https://doi.org/10.1038/s41392-023-01576-4 DOI: https://doi.org/10.1038/s41392-023-01576-4
Johnson, C. H., & Gonzalez, F. J. (2012). Challenges and opportunities of metabolomics. Journal of Cellular Physiology, 227(8), 2975–2981. https://doi.org/10.1002/jcp.24002 DOI: https://doi.org/10.1002/jcp.24002
Kaaks, R., Berrino, F., Key, T., Rinaldi, S., Dossus, L., Biessy, C., Secreto, G., Amiano, P., Bingham, S., Boeing, H., De Mesquita, H. B. B., Chang-Claude, J., Clavel-Chapelon, F., Fournier, A., Van Gils, C. H., Gonzalez, C. A., Gurrea, A. B., Critselis, E., Khaw, K. T., … Riboli, E. (2005). Serum Sex Steroids in Premenopausal Women and Breast Cancer Risk Within the European Prospective Investigation into Cancer and Nutrition (EPIC). JNCI: Journal of the National Cancer Institute, 97(10), 755–765. https://doi.org/10.1093/jnci/dji132 DOI: https://doi.org/10.1093/jnci/dji132
Kamińska, M., Ciszewski, T., Łopacka-Szatan, K., Miotła, P., & Starosławska, E. (2015). Breast cancer risk factors. Menopausal Review, 3, 196–202. https://doi.org/10.5114/pm.2015.54346 DOI: https://doi.org/10.5114/pm.2015.54346
Kanarek, N., Keys, H. R., Cantor, J. R., Lewis, C. A., Chan, S. H., Kunchok, T., Abu-Remaileh, M., Freinkman, E., Schweitzer, L. D., & Sabatini, D. M. (2018). Histidine catabolism is a major determinant of methotrexate sensitivity. Nature, 559(7715), 632–636. https://doi.org/10.1038/s41586-018-0316-7 DOI: https://doi.org/10.1038/s41586-018-0316-7
Kostara, C. E. (2023). Expanding the Molecular Disturbances of Lipoproteins in Cardiometabolic Diseases: Lessons from Lipidomics. Diagnostics, 13(4), 721. https://doi.org/10.3390/diagnostics13040721 DOI: https://doi.org/10.3390/diagnostics13040721
Li, X., Li, J., Hu, Q., Zhang, X., & Chen, F. (2024). Association of physical weight statuses defined by body mass index (BMI) with molecular subtypes of premenopausal breast cancer: A systematic review and meta-analysis. Breast Cancer Research and Treatment, 203(3), 429–447. https://doi.org/10.1007/s10549-023-07139-z DOI: https://doi.org/10.1007/s10549-023-07139-z
Liang, J., Zhang, B., Hu, Y., Na, Z., & Li, D. (2023). Effects of steroid hormones on lipid metabolism in sexual dimorphism: A Mendelian randomization study. Frontiers in Endocrinology, 13, 1119154. https://doi.org/10.3389/fendo.2022.1119154 DOI: https://doi.org/10.3389/fendo.2022.1119154
Lin, C., Tian, Q., Guo, S., Xie, D., Cai, Y., Wang, Z., Chu, H., Qiu, S., Tang, S., & Zhang, A. (2024). Metabolomics for Clinical Biomarker Discovery and Therapeutic Target Identification. Molecules, 29(10), 2198. https://doi.org/10.3390/molecules29102198 DOI: https://doi.org/10.3390/molecules29102198
Liu, Y., & Cao, X. (2016). Characteristics and Significance of the Pre-metastatic Niche. Cancer Cell, 30(5), 668–681. https://doi.org/10.1016/j.ccell.2016.09.011 DOI: https://doi.org/10.1016/j.ccell.2016.09.011
McNamara, K. M., Yoda, T., Takagi, K., Miki, Y., Suzuki, T., & Sasano, H. (2013). Androgen receptor in triple negative breast cancer. The Journal of Steroid Biochemistry and Molecular Biology, 133, 66–76. https://doi.org/10.1016/j.jsbmb.2012.08.007 DOI: https://doi.org/10.1016/j.jsbmb.2012.08.007
Mei, L., Zhang, Z., Li, X., Yang, Y., & Qi, R. (2023). Metabolomics profiling in prediction of chemo-immunotherapy efficiency in advanced non-small cell lung cancer. Frontiers in Oncology, 12, 1025046. https://doi.org/10.3389/fonc.2022.1025046 DOI: https://doi.org/10.3389/fonc.2022.1025046
Meikle, P. J., Wong, G., Barlow, C. K., & Kingwell, B. A. (2014). Lipidomics: Potential role in risk prediction and therapeutic monitoring for diabetes and cardiovascular disease. Pharmacology & Therapeutics, 143(1), 12–23. https://doi.org/10.1016/j.pharmthera.2014.02.001 DOI: https://doi.org/10.1016/j.pharmthera.2014.02.001
Menon, G., Alkabban, F. M., & Ferguson, T. (2025). Breast Cancer. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK482286/
Mimmi, M. C., Picotti, P., Corazza, A., Betto, E., Pucillo, C. E., Cesaratto, L., Cedolini, C., Londero, V., Zuiani, C., Bazzocchi, M., & Esposito, G. (2011). High-performance metabolic marker assessment in breast cancer tissue by mass spectrometry. Cclm, 49(2), 317–324. https://doi.org/10.1515/CCLM.2011.060 DOI: https://doi.org/10.1515/CCLM.2011.060
Miyoshi, Y., Ando, A., Shiba, E., Taguchi, T., Tamaki, Y., & Noguchi, S. (2001). Involvement of up-regulation of 17?-hydroxysteroid dehydrogenase type 1 in maintenance of intratumoral high estradiol levels in postmenopausal breast cancers. International Journal of Cancer, 94(5), 685–689. https://doi.org/10.1002/ijc.1525 DOI: https://doi.org/10.1002/ijc.1525
Moore, D.C. PharmD, Bcps, Bcop, Dpla, Fccp, D., & S. Guinigundo, Msn, Rn, Cnp, Anp-Bc, A. (2023). The Role of Biomarkers in Guiding Clinical Decision-Making in Oncology. Journal of the Advanced Practitioner in Oncology, 14(3), 15–37. https://doi.org/10.6004/jadpro.2023.14.3.17 DOI: https://doi.org/10.6004/jadpro.2023.14.3.17
Park, M., Kim, D., Ko, S., Kim, A., Mo, K., & Yoon, H. (2022). Breast Cancer Metastasis: Mechanisms and Therapeutic Implications. International Journal of Molecular Sciences, 23(12), 6806. https://doi.org/10.3390/ijms23126806 DOI: https://doi.org/10.3390/ijms23126806
Parveen Shaikh, N., Murvanidze, I., Shaikh, A. P., Khurana, R., & Nakashidze, I. (2023). The Altered Gene Expression and Epigenetic Mechanisms in Breast Cancer. Journal of Biomedical Research & Environmental Sciences, 4(10), 1461–1469. https://doi.org/10.37871/jbres1819 DOI: https://doi.org/10.37871/jbres1819
Passaro, A., Al Bakir, M., Hamilton, E. G., Diehn, M., André, F., Roy-Chowdhuri, S., Mountzios, G., Wistuba, I. I., Swanton, C., & Peters, S. (2024). Cancer biomarkers: Emerging trends and clinical implications for personalized treatment. Cell, 187(7), 1617–1635. https://doi.org/10.1016/j.cell.2024.02.041 DOI: https://doi.org/10.1016/j.cell.2024.02.041
Perou, C. M., Sørlie, T., Eisen, M. B., Van De Rijn, M., Jeffrey, S. S., Rees, C. A., Pollack, J. R., Ross, D. T., Johnsen, H., Akslen, L. A., Fluge, Ø., Pergamenschikov, A., Williams, C., Zhu, S. X., Lønning, P. E., Børresen-Dale, A.-L., Brown, P. O., & Botstein, D. (2000). Molecular portraits of human breast tumours. Nature, 406(6797), 747–752. https://doi.org/10.1038/35021093 DOI: https://doi.org/10.1038/35021093
Petan, T. (2020). Lipid Droplets in Cancer. In S. H. F. Pedersen & D. L. Barber (Eds.), Organelles in Disease (Vol. 185, pp. 53–86). Springer International Publishing. https://doi.org/10.1007/112_2020_51 DOI: https://doi.org/10.1007/112_2020_51
Petrović, N., Nakashidze, I., & Nedeljković, M. (2021). Correction to: Breast Cancer Response to Therapy: Can microRNAs Lead the Way? Journal of Mammary Gland Biology and Neoplasia, 26(2), 179–179. https://doi.org/10.1007/s10911-021-09480-9 DOI: https://doi.org/10.1007/s10911-021-09480-9
Petrovic, N., Sami, A., Martinovic, J., Zaric, M., Nakashidze, I., Lukic, S., & Jovanovic-Cupic, S. (2017). TIMP-3 mRNA expression levels positively correlates with levels of miR-21 in in situ BC and negatively in PR positive invasive BC. Pathology - Research and Practice, 213(10), 1264–1270. https://doi.org/10.1016/j.prp.2017.08.012 DOI: https://doi.org/10.1016/j.prp.2017.08.012
Possemato, R., Marks, K. M., Shaul, Y. D., Pacold, M. E., Kim, D., Birsoy, K., Sethumadhavan, S., Woo, H.-K., Jang, H. G., Jha, A. K., Chen, W. W., Barrett, F. G., Stransky, N., Tsun, Z.-Y., Cowley, G. S., Barretina, J., Kalaany, N. Y., Hsu, P. P., Ottina, K., Chan, A.M., Yuan, B., Garraway, L.A., Root, D.E., Mino-Kenudson, M., Brachtel, E.F., Driggers, E.M., & Sabatini, D. M. (2011). Functional genomics reveal that the serine synthesis pathway is essential in breast cancer. Nature, 476(7360), 346–350. https://doi.org/10.1038/nature10350 DOI: https://doi.org/10.1038/nature10350
Prat, A., Pineda, E., Adamo, B., Galván, P., Fernández, A., Gaba, L., Díez, M., Viladot, M., Arance, A., & Muñoz, M. (2015). Clinical implications of the intrinsic molecular subtypes of breast cancer. The Breast, 24, S26–S35. https://doi.org/10.1016/j.breast.2015.07.008 DOI: https://doi.org/10.1016/j.breast.2015.07.008
Rajkumar, T., Amritha, S., Sridevi, V., Gopal, G., Sabitha, K., Shirley, S., & Swaminathan, R. (2022). Identification and validation of plasma biomarkers for diagnosis of breast cancer in South Asian women. Scientific Reports, 12(1), 100. https://doi.org/10.1038/s41598-021-04176-w DOI: https://doi.org/10.1038/s41598-021-04176-w
Reis, G. B., Rees, J. C., Ivanova, A. A., Kuklenyik, Z., Drew, N. M., Pirkle, J. L., & Barr, J. R. (2021). Stability of lipids in plasma and serum: Effects of temperature-related storage conditions on the human lipidome. Journal of Mass Spectrometry and Advances in the Clinical Lab, 22, 34–42. https://doi.org/10.1016/j.jmsacl.2021.10.002 DOI: https://doi.org/10.1016/j.jmsacl.2021.10.002
Roshanzamir, F., Robinson, J. L., Cook, D., Karimi-Jafari, M. H., & Nielsen, J. (2022). Metastatic triple negative breast cancer adapts its metabolism to destination tissues while retaining key metabolic signatures. Proceedings of the National Academy of Sciences, 119(35), e2205456119. https://doi.org/10.1073/pnas.2205456119 DOI: https://doi.org/10.1073/pnas.2205456119
Rossi, C., Cicalini, I., Cufaro, M. C., Consalvo, A., Upadhyaya, P., Sala, G., Antonucci, I., Del Boccio, P., Stuppia, L., & De Laurenzi, V. (2022). Breast cancer in the era of integrating “Omics” approaches. Oncogenesis, 11(1), 17. https://doi.org/10.1038/s41389-022-00393-8 DOI: https://doi.org/10.1038/s41389-022-00393-8
Russo, J., & Russo, I. H. (2006). The role of estrogen in the initiation of breast cancer. The Journal of Steroid Biochemistry and Molecular Biology, 102(1–5), 89–96. https://doi.org/10.1016/j.jsbmb.2006.09.004 DOI: https://doi.org/10.1016/j.jsbmb.2006.09.004
Salciccia, S., Capriotti, A. L., Laganà, A., Fais, S., Logozzi, M., De Berardinis, E., Busetto, G. M., Di Pierro, G. B., Ricciuti, G. P., Del Giudice, F., Sciarra, A., Carroll, P. R., Cooperberg, M. R., Sciarra, B., & Maggi, M. (2021). Biomarkers in Prostate Cancer Diagnosis: From Current Knowledge to the Role of Metabolomics and Exosomes. International Journal of Molecular Sciences, 22(9), 4367. https://doi.org/10.3390/ijms22094367 DOI: https://doi.org/10.3390/ijms22094367
Sánchez-Castillo, A., & Kampen, K. R. (2024). Understanding serine and glycine metabolism in cancer: A path towards precision medicine to improve patient’s outcomes. Discover Oncology, 15(1), 652. https://doi.org/10.1007/s12672-024-01544-6 DOI: https://doi.org/10.1007/s12672-024-01544-6
Schramm, A., De Gregorio, N., Widschwendter, P., Fink, V., & Huober, J. (2015). Targeted Therapies in HER2-Positive Breast Cancer—A Systematic Review. Breast Care, 10(3), 173–178. https://doi.org/10.1159/000431029 DOI: https://doi.org/10.1159/000431029
Shahisavandi, M., Wang, K., Ghanbari, M., & Ahmadizar, F. (2023). Exploring Metabolomic Patterns in Type 2 Diabetes Mellitus and Response to Glucose-Lowering Medications—Review. Genes, 14(7), 1464. https://doi.org/10.3390/genes14071464 DOI: https://doi.org/10.3390/genes14071464
Smolarz, B., Nowak, A. Z., & Romanowicz, H. (2022). Breast Cancer—Epidemiology, Classification, Pathogenesis and Treatment (Review of Literature). Cancers, 14(10), 2569. https://doi.org/10.3390/cancers14102569 DOI: https://doi.org/10.3390/cancers14102569
Snell, C. E., Gough, M., Liu, C., Middleton, K., Pyke, C., Shannon, C., Woodward, N., Hickey, T. E., Armes, J. E., & Tilley, W. D. (2018). Improved relapse-free survival on aromatase inhibitors in breast cancer is associated with interaction between oestrogen receptor-α and progesterone receptor-b. British Journal of Cancer, 119(11), 1316–1325. https://doi.org/10.1038/s41416-018-0331-3 DOI: https://doi.org/10.1038/s41416-018-0331-3
Soori, M., Platz, E. A., Brawley, O. W., Lawrence, R. S., & Kanarek, N. F. (2022). Inclusion of the US Preventive Services Task Force Recommendation for Mammography in State Comprehensive Cancer Control Plans in the US. JAMA Network Open, 5(5), e229706. https://doi.org/10.1001/jamanetworkopen.2022.9706 DOI: https://doi.org/10.1001/jamanetworkopen.2022.9706
Sun, C., Wang, A., Zhou, Y., Chen, P., Wang, X., Huang, J., Gao, J., Wang, X., Shu, L., Lu, J., Dai, W., Bu, Z., Ji, J., & He, J. (2023). Spatially resolved multi-omics highlights cell-specific metabolic remodeling and interactions in gastric cancer. Nature Communications, 14(1), 2692. https://doi.org/10.1038/s41467-023-38360-5 DOI: https://doi.org/10.1038/s41467-023-38360-5
Suri, G. S., Kaur, G., Carbone, G. M., & Shinde, D. (2023). Metabolomics in oncology. Cancer Reports, 6(3), e1795. https://doi.org/10.1002/cnr2.1795 DOI: https://doi.org/10.1002/cnr2.1795
Suzuki, T., Miki, Y., Moriya, T., Akahira, J., Hirakawa, H., Ohuchi, N., & Sasano, H. (2007). In situ production of sex steroids in human breast carcinoma. Medical Molecular Morphology, 40(3), 121–127. https://doi.org/10.1007/s00795-007-0365-8 DOI: https://doi.org/10.1007/s00795-007-0365-8
Takagi, K., Miki, Y., Nagasaki, S., Hirakawa, H., Onodera, Y., Akahira, J., Ishida, T., Watanabe, M., Kimijima, I., Hayashi, S., Sasano, H., & Suzuki, T. (2010). Increased intratumoral androgens in human breast carcinoma following aromatase inhibitor exemestane treatment. Endocrine-Related Cancer, 17(2), 415–430. https://doi.org/10.1677/ERC-09-0257 DOI: https://doi.org/10.1677/ERC-09-0257
Talarico, M. C. R., Derchain, S., Da Silva, L. F., Sforça, M. L., Rocco, S. A., Cardoso, M. R., & Sarian, L. O. (2024). Metabolomic Profiling of Breast Cancer Patients Undergoing Neoadjuvant Chemotherapy for Predicting Disease-Free and Overall Survival. International Journal of Molecular Sciences, 25(16), 8639. https://doi.org/10.3390/ijms25168639 DOI: https://doi.org/10.3390/ijms25168639
Tan, B., Zhang, Y., Zhang, T., He, J., Luo, X., Bian, X., Wu, J., Zou, C., Wang, Y., & Fu, L. (2020). Identifying potential serum biomarkers of breast cancer through targeted free fatty acid profiles screening based on a GC–MS platform. Biomedical Chromatography, 34(10), e4922. https://doi.org/10.1002/bmc.4922 DOI: https://doi.org/10.1002/bmc.4922
Tilson-Mallett, N., Santner, S. J., Feil, P. D., & Santen, R. J. (1983). Biological Significance of Aromatase Activity in Human Breast Tumors*. The Journal of Clinical Endocrinology & Metabolism, 57(6), 1125–1128. https://doi.org/10.1210/jcem-57-6-1125 DOI: https://doi.org/10.1210/jcem-57-6-1125
Valko-Rokytovská, M., Očenáš, P., Salayová, A., & Kostecká, Z. (2021). Breast Cancer: Targeting of Steroid Hormones in Cancerogenesis and Diagnostics. International Journal of Molecular Sciences, 22(11), 5878. https://doi.org/10.3390/ijms22115878 DOI: https://doi.org/10.3390/ijms22115878
Van Den Brandt, P. A., Ziegler, R. G., Wang, M., Hou, T., Li, R., Adami, H.-O., Agnoli, C., Bernstein, L., Buring, J. E., Chen, Y., Connor, A. E., Eliassen, A. H., Genkinger, J. M., Gierach, G., Giles, G. G., Goodman, G. G., Håkansson, N., Krogh, V., Le Marchand, L., Lee, I.M., Liao, L.M., Martinez, M.E., Miller, A.B., Milne, R.L., Neuhouser, M.L., Patel, A.V., Prizment, A., Robien, K., Rohan, T.E., Sawada, N., Schouten, L.J., Sinha, R., Stolzenberg-Solomon, R.Z., Teras, L.R., Tsugane, S., Visvanathan, K., Weiderpass, E., White, K.K., Willett, W.C., Wolk, A., Zeleniuch-Jacquotte, A., & Smith-Warner, S. A. (2021). Body size and weight change over adulthood and risk of breast cancer by menopausal and hormone receptor status: A pooled analysis of 20 prospective cohort studies. European Journal of Epidemiology, 36(1), 37–55. https://doi.org/10.1007/s10654-020-00688-3 DOI: https://doi.org/10.1007/s10654-020-00688-3
Veerla, S., Hohmann, L., Nacer, D. F., Vallon-Christersson, J., & Staaf, J. (2023). Perturbation and stability of PAM50 subtyping in population-based primary invasive breast cancer. Npj Breast Cancer, 9(1), 83. https://doi.org/10.1038/s41523-023-00589-0 DOI: https://doi.org/10.1038/s41523-023-00589-0
Vinogradova, Y., Coupland, C., & Hippisley-Cox, J. (2020). Use of hormone replacement therapy and risk of breast cancer: Nested case-control studies using the QResearch and CPRD databases. BMJ, m3873. https://doi.org/10.1136/bmj.m3873 DOI: https://doi.org/10.1136/bmj.m3873
Wagner-Golbs, A., Neuber, S., Kamlage, B., Christiansen, N., Bethan, B., Rennefahrt, U., Schatz, P., & Lind, L. (2019). Effects of Long-Term Storage at −80 °C on the Human Plasma Metabolome. Metabolites, 9(5), 99. https://doi.org/10.3390/metabo9050099 DOI: https://doi.org/10.3390/metabo9050099
Yang, K., & Han, X. (2016). Lipidomics: Techniques, Applications, and Outcomes Related to Biomedical Sciences. Trends in Biochemical Sciences, 41(11), 954–969. https://doi.org/10.1016/j.tibs.2016.08.010 DOI: https://doi.org/10.1016/j.tibs.2016.08.010
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Ahishtan Febrian Nishanthan, Ermira Jahja, Tamar Peshkova, Nameera Parveen Shaikh, Aleena Parveen Shaikh, Joy Dip Barua, Irina Nakashidze

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.